For this edition of “C-suite Conversations” I had the honor of interviewing my long-time friend and industry colleague, Dr. John Glaser. John’s career in healthcare IT has been illustrative and impressive, to say the least. He is currently an Executive-in-Residence at Harvard Medical School. Previously, he served as CIO of Brigham and Women’s Hospital for over seven years, and CIO of Partners HealthCare for 15 years. He was also SVP of Population Health at Cerner and CEO of Siemens Health Services. John was the founding chair of the College of Healthcare Information Management Executives (CHIME), he is a past president of the Healthcare Information and Management Systems Society (HIMSS), and he has served on numerous boards. Read his full bio here.
Key Takeaways
- Establish clear accountability structures when creating multiple C-level technology positions – having numerous chief officers (CISO, CMIO, CDO) can create confusion about decision-making authority, especially during vendor issues or major initiatives.
- Prioritize core leadership skills over technical expertise when selecting technology leaders – this includes strategic thinking, communication abilities, and team-building capabilities.
- Focus on senior executive capabilities first and technical knowledge second when hiring technology leaders – seek candidates who can effectively move organizations forward, motivate teams, and maintain emotional stability while understanding the technology landscape.
Q & A with John
Judy Kirby: John, you are an icon in the healthcare technology profession. First, I want to thank you for all the contributions you have made to the industry over the years. You and I have known each other longer than either of us care to admit at this point. And we’ve witnessed a lot of changes – changes you have influenced. But first, how did you get into healthcare technology?

Dr. John Glaser: Thank you, Judy. Like a lot of careers, my path was not a direct shot. When I got out of college in 1976, I had a degree in math and no idea what to do. So, I worked at Pizza Hut, I worked in a salmon cannery, and in my big life adventure, I hitchhiked from Fairbanks, Alaska to the Panama Canal. It took me six months. Six months is a long time, and I missed this woman whom I was madly in love with, who I’d met back at Durham, North Carolina.
So, I went back to Durham and took the first job I was offered as a programmer analyst at Research Triangle Institute, which was doing a study of national medical care expenditures and quality. So, I randomly stumbled into healthcare by following my heart, and 50 years later I am still together with both the healthcare industry and the woman, Denise.
I thought healthcare was pretty darn cool but I didn’t really want to be a programmer for the rest of my life. My stepmother suggested I go and get a Ph.D. in medical informatics. So, Denise and I got married and went off to the University of Minnesota, where I spent four years getting overly educated in medical informatics, which led to becoming head of the healthcare IT consulting practice at Arthur D. Little.
JK: Years ago, you and I presented at CHIME on the evolution of the CIO. But today we see so many new titles. What are the major differences between the titles of chief data officer, chief digital information officer, and CIO? How do you feel about spreading technology across many different people?
JG: I became CIO at the Brigham and Women’s Hospital in 1988. At the time, the CIO job title was becoming common in other industries but not so much in healthcare. It was relatively new for the boards of healthcare systems and for CEOs. But IT has evolved a lot from a cost center to being viewed much more as a strategic asset. There’s no question on the part of leadership that there is strategic value in IT.
Now there are all these chief officer roles – chief information security officer, chief medical information officer, chief nursing officer. Now there’s a Chief AI officer. On the one hand, if you really want to attract talent, sometimes you have to put this fancy title on it. I get that. But I do think it runs the huge risk, and I actually wrote an article a couple of years ago about having too many chiefs.
With so many chiefs, the accountability becomes a little murky. If we have a Chief Medical Information Officer, CIO, and a Chief Analytics Officer, and there is a major issue with a vendor, who deals with that? Who’s fundamentally accountable for certain relationships? So, I think it’s okay to have chiefs, but you better be sure you keep the accountability structure clear about who gets to make what decisions.
JK: I would agree with you. Something I have seen recently is the top IT person is now titled Chief Technology Officer. It’s gone from the CTO reporting to the CIO to the CTO being the top IT role.
JG: Chief Information Officer is a little fuzzy. What are you in charge of, information? How does that work? Information is everywhere. The traditional role of CTO was the tech wizard. They made sure that the architecture was solid, that the interoperability was as good as it could be, and that things were secure. So, if one views it as a technical role, and that the top person should be a technical person, that could be a mistake because it’s broader than that. They’re functioning as a change leader, strategist and business expert.
Call them whatever you want, but you have to be careful with how it is perceived externally and internally. You run the risk of confusing the rest of the organization, and you run the risk that, as you’re trying to attract talent, they will read certain things into the title that you don’t intend. Make it clear what the role does, and be sure the actual title doesn’t demean, diminish, or narrow the perception of the job.
JK: Whatever the title, how do you see the top IT officer role evolving over the next three to five years? What might some new responsibilities or job qualifications be?
JG: In a way, Judy, the qualifications and the skills are the same ones that you and I were talking about 20 years ago. You want someone who has good strategic instincts. You want someone who communicates well with the clinical leaders. You want someone who builds great teams and motivates them to do amazing things. You want somebody who’s got an astute read of the technology and is not overwhelmed by fatuous sayings. All of that is the same. You have to know new things that you didn’t have to know about before, like AI and value-based care, but the human skills needed are generally the same.
I do think that the bar continues to get raised. So, if you got an A grade as a CIO 10 years ago, today you’re going to get a B. The bar is raised in terms of the skill and the prowess. It’s just harder, it is more demanding, it requires that you communicate more effectively than you did before. It requires that you have a better performing team than you did before. Things that need to get done are more significant, more strategically critical, and frankly, you’re more resource constrained. You have to operate with less budget than you had before. So, in many ways the role is the same as before but it is much more demanding.
JK: I agree. The average turnover of healthcare CIOs has been somewhere between three and four years for a long time. Why such high turnover?
JG: I think it is not all that different from CEO or CFO turnover. I suspect a couple of things happen. One is that as a CIO, you can make a wrong call for which the results are more dramatic. You know, one bad implementation and “Adios.” One security breach and it can all be all over in a hurry. A CIO’s bad call is much more dramatic and obvious than when a CEO misses a call on strategy.
But nonetheless, people burn out. They think, “I’ve done what I wanted to do here, and as a careerist, I want to try something different.” They get kind of tired and stale at a level, particularly people who are ambitious and who want to climb ladders.
JK: One of the big concerns I hear repeatedly, and we see it in our search business, is the lack of up-and-coming IT leaders to fill future healthcare CIO positions. What are your thoughts around this void, and how do we fix it?
JG: We see that issue in multiple parts of our economy. For example, there’s a shortage of primary care providers. How do you persuade people to become primary care providers? Well there’s a lot of reasons why that’s hard, or they want to go off and make more money as a specialist, etc.
I don’t know what we do here. You have to tap into the people who want to be in IT and healthcare because it’s interesting. It’s got some significant challenges, and many people want to do good in the world. They want their lives to have meaning and help people who are sick or dying or going through tough times health-wise. This is largely a nonprofit industry so you are competing with the golden riches of stock options, which may or may not happen, but they’re still enticing.
Healthcare has some things going for it, but still, you have to reach a 22-year-old who’s in college or someone who’s 25 and maybe doing banking and IT stuff. Once you get them in, you can see who wants to climb the management ladder, who is good at it, and who thrives on it. You ask a good question. I don’t know what the answer is.
JK: Looking back at your own journey, what career advice do you have for rising healthcare technology professionals interested in becoming a CIO one day?
JG: You have to decide that you really like leadership and management and that you enjoy motivating people. It’s very paternal because the victories are in what they do, not what you do. It’s like watching your kids do great things. I like running things, and I like the paternal feeling, and I like helping people go left versus right.
The other advice is to seek out role models. I remember going to medical informatics conferences when I was in graduate school and seeing a panel up there with all the legends of the field: Clem McDonald, Octo Barnett, the first pioneers of medical informatics, and thinking, “Wow, they’re really smart, and some of them are really funny, and they’re really competent. I want to be like them.” It’s fine to let them know it, to go up to them and say, I admire and respect you. Would you talk to me from time to time?” People warm up to that.
JK: Great advice! Anything else?
If you hit a ceiling, try another organization. I also think it’s fair to take reasonable risks. Don’t bet the farm and don’t bet your life savings, but it’s okay to try things that you’re not sure you can do and that you might screw up. In the grand scheme of things, if you get fired, no big deal. People survive that, and it is nothing compared to other calamities like having a sick kid.
JK: Where do you see generative AI having the most impact in healthcare over the next three to five years?
JG: I don’t know. I had an interesting conversation with some Scottsdale Institute CEOs from large health systems a couple of weeks ago about where they are with GenAI. They’re all experimenting with it at various levels – ambient listening, where the computer creates notes, some revenue cycle coding. But I wouldn’t characterize these as transformative.
I think what’s needed now is a set of ideas on the table which really could change the game, and we’ll have to see whether those play. So, I’ll give you an example. I sit on the board of National Committee for Quality Assurance (NCQA). I’m the incoming chairman of the board, and as you know, they do Healthcare Effectiveness Data and Information Set (HEDIS) measures, the methodology by which to measure various aspects of care. Well, how does that methodology work? They convene a room full of blue-ribbon clinicians, and they feed them lots of articles, and they arm wrestle, and several weeks later out comes an answer. An example answer might be the best way to measure the quality of prenatal care. It’s a process that works but it’s slow and it’s expensive to do this way. How about we have GenAI scan the literature and offer up a draft, then the committee debate the draft? Wow, that’s different. You might do that in minutes versus weeks.
As another example, of AI (although AI that is deep learning) a health plan can go through a range of diseases, and we believe that for every 100 subscribers, roughly one third will get vaccinated. We don’t have to do anything, they just will. And another third, they’re not going to get it for whatever reason no matter what we do. It’s the middle third, the persuadable ones who, if we play it the right way, will tilt. The question is, who are they? So, using algorithms to identify and target that one third would be much more precise and personalized. We see this already in retail. It’s unbelievable. My kid, the middle kid, is the VP of Consumer Analytics for a large department store chain and they are really all over this stuff.
I think we’ll also use AI to personalize care perhaps to identify treatments that are more effective than others.
I think one of the other things to remember is – how long has the internet been around? I mean commercially. Google was founded in 1998, that’s 26 years. On one hand, we have seen an amazing range of uses in a very short period of time. On the other hand, the web is still evolving in our lives.
So, you can look for ideas that are three to five years out but I think the question is also how will AI affect society for decades. There is this rolling horizon of new things coming that will never stop. Even 20 years from now, we’ll always discover new ways to leverage the technology.
JK: What advice would you give to CEOs about hiring their next technology leader?
JG: I think it’s the same advice I would give them if they’re hiring their next CFO, or their next chief medical officer, or their next chief human resources officer. You need a senior executive who functions and acts like a senior executive. They’re smart, they’re articulate, they communicate. They have an emotional even keel, and they know how to pull together teams. You want someone who’s skilled at moving an organization and motivating people, but you also want them to possess a knowledge base. With the CFO, you want that person to understand the ways you can borrow money. With the chief medical officer, you want someone conversant with, for example, GLP-1s, and the issues confronting the medical staff. You want the same in your CIO – someone who understands the technology and can sit with you and have a conversation. When you ask a candidate what they think about GenAI, you better get a pretty articulate answer, that you can relate to and understand.
JK: Right. If you hadn’t become an IT leader, what other career do you think you were cut out for?
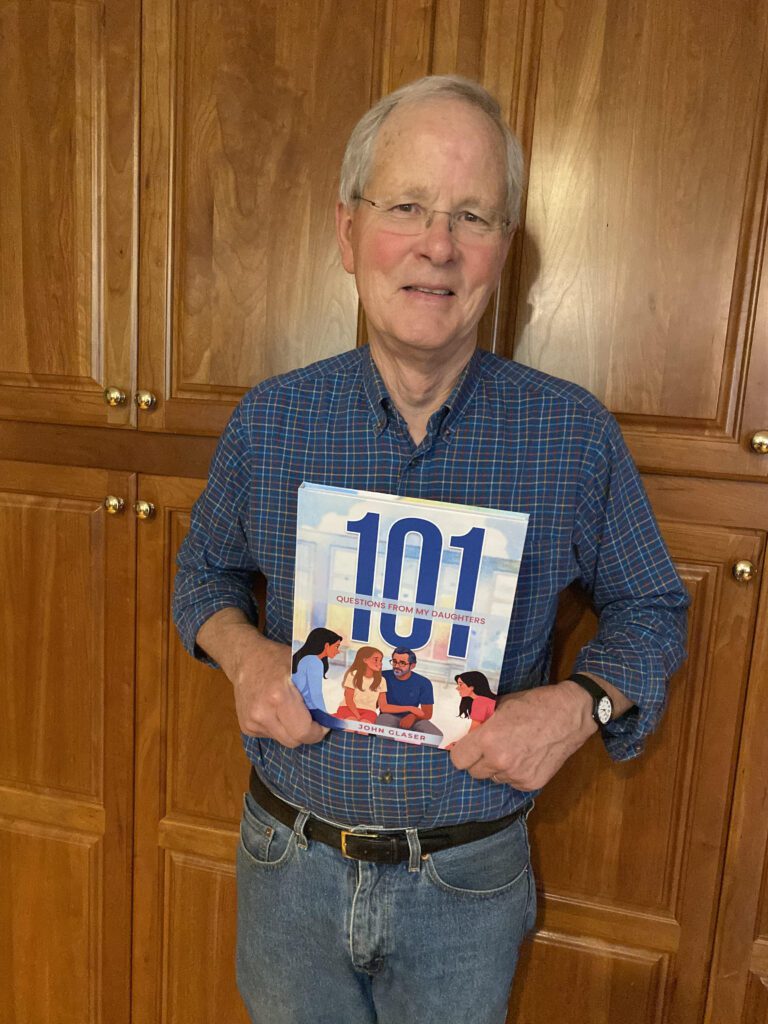
JG: I don’t know. It’s a fair question. I like the leadership thing a lot. I think that’s fun. And I like teaching a lot. I do a lot of executive education these days and I really enjoy that. And I like writing a lot. I wrote a book, 101 Questions My Daughters Asked Me. They asked me “What does love mean to you?” “What were you like as a teenager?” “What supported you in life?” I like the healthcare field because it’s real. My father died of Lewy body disease, and my younger brother has it now. There are people in my family who have encountered the healthcare system when they are very sick. So, there’s a reality here, and I’d like to think that I’m helping make it better.
I like the fact that technology can enable you to do things which are really impressive. I remember CPOE (Computer Provider Order Entry) back in the day and how it significantly reduced medication errors at the Brigham. That was really cool! That’s why we’re here. So, for someone like me who likes leading people, likes the world to have meaning, likes writing, likes teaching, and likes the power of ideas, what other roles are there? I wouldn’t be a professional basketball player. I’m not sure I’d want to be a lawyer, or a doctor. I would be something in the general management realm, although maybe not as much IT. We’ll just have to see, although my career is largely winding down at this point.
JK: So outside of work and spending time with friends and family, what’s something you love to do when you have time?

JG: I write a letter to my family every week now for 35 years, four pages long. I love to do that. And I will be reading some children’s stories I wrote for Emma, my granddaughter, to her kindergarten class in a couple of weeks.
Like a lot of folks who are in the later years of their careers, we are traveling. We were in Scotland back in September, we’ll be in Scandinavia in May. We spend a fair amount of time on Cape Cod. I probably work about half the time, and the rest of the time is writing, getting in my 10,000 steps a day, hanging out with grandkids, some traveling, the usual mix of stuff that is not uncommon when you’re in your late 60s.